How Does Hormonal Birth Control Work?

Hormonal contraceptives havecome a looooong way since they first became available in the 1950s. The contraception of yesteryear looked different, too—both because the Pill itself has evolved so much, and because options have expanded immensely. Many women aren’t even aware of their many choices or know much about them, says Jennifer L. Lew, M.D., OB/GYN at Northwestern Medicine Regional Medical Group in Chicago, IL. And the more we know, the better equipped we are to make decisions that fit our lifestyles, health, and family planning goals. Here, experts give the 411 on hormonal birth control.

How Progestin in the Pill Works
主要有两种激素用于避孕pills: progestin and estrogen. Progestin is a synthetic (meaning, man-made) form of progesterone, a hormone that naturally occurs in the body and plays an important role in menstruation and pregnancy. The doses used in birth control do two main things to prevent pregnancy. First, progestin interferes with signals in the brain that tell the ovaries to produce follicles and, ultimately, eggs. Progestin also thickens the mucus in the cervix, making it difficult for sperm to travel up into the fallopian tubes and fertilize any available eggs.

The Role of Estrogen in the Pill
Hormonal birth control may also contain a synthetic form of estrogen. Estrogen’s main role is to counteract side effects of progestin, explains Mitchell D. Creinin, M.D., an OB/GYN and family planning expert at UC Davis Health in Sacramento, CA. “At a low dose, progestin thickens mucus but does not shut off the ovaries. Higher dosages shut off the ovaries but also shut off other hormones, including estrogen, which you need to keep your hormones balanced,” Dr. Creinin explains, and prevent the side effects of low estrogen, which can include moodiness, reduced energy, trouble sleeping, and even hot flashes or decreased sex drive.

The Pill Has Changed Over Time
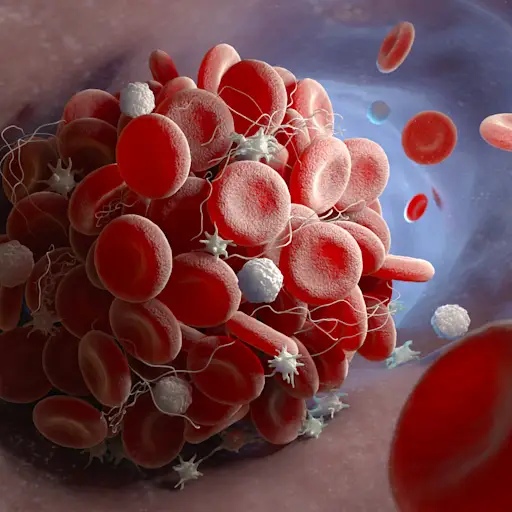
When birth control came out in the ‘50s, it hada lotof estrogen in it. According to the (online only) Museum of Menstruation and Women’s Health, the first marketed pill, Enovid 10, contained 9.85 mg of progestin (norethynodrel) and 150 micrograms (μg) of estrogen (mestranol). Modern pills only contain between 0.1 to 3.0 mg of progestin and 20 to 50 μg of estrogens. That’s because we’ve developed better progestins that do the job with a drastically smaller dosage. Plus, we’ve learned more about the potential risks of too much estrogen, including blood clots and breast and cervical cancer.
Consider Your Existing Health Issues
Combined contraceptives like the Pill and the patch are not recommended for people with uncontrolledhypertension, smokers over 35, and anyone with a history of blood clots, ischemicheart disease、偏头痛和光环或活跃(or history of) breast or endometrial cancer and valvular heart disease. There are estrogen-free contraception options available that are much safer for these populations. The combination birth control pill is associated with an increased risk of blood clots in all women, but the risk is relatively low—lower than the risk of blood clots during pregnancy—if you don’t have any of the above conditions.

There Are Estrogen-Free Options
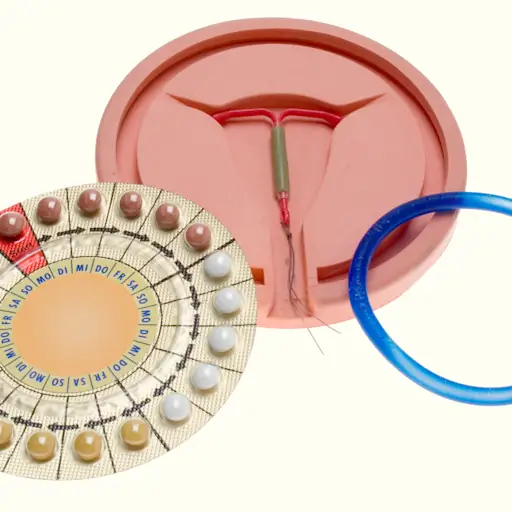
Hormonal IUDs and the implant are two estrogen-free hormonal birth control options. And it just so happens that these are considered to be the most effective forms of reversible birth control available. Over time, long-acting reversible contraceptives (LARCs) are 20 times more effective than birth control pills, the patch, or the ring, according to the American College of Obstetricians and Gynecologists (ACOG). Hormonal IUDs may cause spotting and increase bleeding at first, but over time, both bleeding and menstrual cramps usually decrease. The implant can also cause changes in bleeding, the most common change being unpredictable bleeding.

The Progestin-Only Mini Pill Is Also Available
There are two types of progestin-only pills—one containing the progestin norethidrone and the other, drospirenone. The norethidrone pill has to be taken at the exact same time each day—if you’re three hours late or more, you need to use backup contraception for two days, since this type of progestin doesn’t stay in your body for very long and uses a lower dose of the hormone, Dr. Creinin explains. The drospirenone pill stays in the body longer, so it has a larger margin for error. (For the regular combo pill, backup is only needed if you miss the right timing for two days in a row.)

So Is the Progestin-Only Shot
Another estrogen-free contraceptive is the progestin-only injection. According to the ACOG, your OB/GYN gives you the jab, and it’s most effective when it’s given every 13 weeks. Shots can be given up to two weeks late (meaning, no more than 15 weeks after your last injection). The injection is slightly more effective than the progestin-only pill; when used perfectly, fewer than one in 100 women get pregnant, according to the ACOG. Both the mini pill and the injection can cause irregular bleeding. The shot is associated with anywhere from minor to significant weight gain and may also cause bone loss over time.
Dosage and Delivery of Hormones Matters
With so many hormonal birth control options, ranging from the Pill, mini pill, patch, IUDs, implant, vaginal rings, and injection, it’s important to know their different delivery methods, how they contain different amounts of hormones, and provide different instructions for use, Dr. Lew says. For example, LARCs like the implant and hormonal IUDs have hormones embedded in them using a slow delivery system that releases them into the uterus or blood stream over multiple years. The ring disperses hormones into the vaginal lining; and the Pill works systemically through the digestive system.
Find Balance Between Efficacy and Side Effects
激素避孕药的副作用是不同的method, but across all types, changes in bleeding can occur, as can headache, breast tenderness, and nausea. Usually, systemic contraceptives like the Pill and the patch tend to cause more side effects than similar combination methods that work locally, like the ring, Dr. Creinin says. The hormonal IUD delivers only progestin locally to the uterus, so the amount that travels throughout the body is very small, reducing the risk of side effects, he adds. Some women find other IUD side effects, like cramping and irregular bleeding, to be intolerable.

Some Trial and Error May Be Required
With multiple options across categories—especially among pills and IUDs—it might take some trial and error to find what’s best for you. “Patients say their body doesn’t tolerate the hormones, but we have to look at how they’re delivered,” Dr. Creinin says. Just because a systematic method like the Pill or patch doesn’t work for you doesn’t mean that other methods with a different mix of hormones and a different delivery method will have the same side effects, he adds. Even a different medication in the same category might make all the difference for you.

Using Birth Control as Prescribed Is Key
Practitioners always want to prescribe whatever birth control method will lead to the highest rate of compliance, Dr. Lew says. Any medication that needs to be taken less frequently generally has higher compliance. That’s why most OB/GYNs recommend IUDs for people who don’t plan to get pregnant for at least a few years. “You can get an IUD in and forget about it for years and years, and it’ll still be working for you,” Dr. Lew says. The downside is that you lose some control because you do have to get it removed by a healthcare provider, Dr. Creinin adds.
How Progestin Works:Statpearls. (2021.) “Oral Contraceptive Pills.”https://www.ncbi.nlm.nih.gov/books/NBK430882/
History of The Pill:The Museum of Menstruation and Women's Health. (2008.) “Enovid-E Birth Control Pills.”http://www.mum.org/enovid-e.htm
The Progestin-Only Pill and Shot:The American College of Obstetricians and Gynecologists. (2020.) “Progestin-Only Hormonal Birth Control: Pill and Injection.”https://www.acog.org/womens-health/faqs/progestin-only-hormonal-birth-control-pill-and-injection
Comparing Progestin-Only and Combined Pills:Centers for Disease Control and Prevention. (2013.) “Recommended Actions After Late or Missed Combined Oral Contraceptives.”https://www.cdc.gov/reproductivehealth/unintendedpregnancy/pdf/248124_fig_2_3_4_final_tag508.pdf
Long-Acting Reversible Contraceptives (LARCs):The American College of Obstetricians and Gynecologists. (2020.) “Long-Acting Reversible Contraception (LARC): Intrauterine Device (IUD) and Implant.”https://www.acog.org/womens-health/faqs/long-acting-reversible-contraception-iud-and-implant
Important Contraindications Of Hormonal Birth Control:StatPearls. (2021.) “Oral Contraceptive Pills.”https://www.ncbi.nlm.nih.gov/books/NBK430882/
Comparing Blood Clot Risk In Pregnancy:Canadian Family Physician. (2012.) “Half a century of the oral contraceptive pill.”https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3520685/
Amy is a freelance journalist and certified personal trainer. She covers a wide range of health topics, including fitness, health conditions, mental health, sexual and reproductive health, nutrition, and more. Her work has appeared on SELF, Bicycling, Health, and other publications. When she's not busy writing or editing, you can find her hiking, cooking, running, or lounging on the couch watching the latest true crime show on Netflix.


